Abstract
For thousands of years, Chinese medicine and conventional Western medicine appeared to be two unrelated and uncompromising paradigms. The history of acupuncture can be traced back for more than 2500 years but today we can use advanced technology to understand ancient healing methods. Acupuncture should not be used to compete with efficacious treatment modalities that are already available in conventional Western medicine. Exploration of its clinical applications should focus on conditions for which conventional medicine can find no satisfactory remedy.
The history of acupuncture can be traced back for more than 2500 years. In Huaungdi Neijing (The Emperor’s Classic of Internal Medicine), a Chinese medical classic compiled between 800 and 300 BC, the techniques and clinical applications of acupuncture were already well described. Yet interest in acupuncture was spawned in the Western world only after the historical visit of President Richard Nixon to the People’s Republic of China in 1972. During this trip one of the reporters from the New York Times underwent emergency appendectomy in China and suffered from post-surgical paralytic ileus. His problem was “miraculously” resolved by acupuncturists in China. Since then the use of acupuncture in anesthesia has been reported in the Western literature.1,2 The use of alternative medicine, including acupuncture, has exploded in the past three decades.
Does acupuncture work? Is it built on robust science and solid clinical evidence? What is the role of acupuncture in gastrointestinal disorders? Is it a myth or a magic remedy? As a medical practitioner brought up in a traditional Chinese family but educated in the classical British medical system in Hong Kong, I must admit that I have both my passion as well as my skepticism for Chinese medicine and acupuncture.
“Whereas Western medicine deals with causative agents of disease entities and specific treatments, Chinese medicine adopts a holistic approach, with the aim of maintaining health by restoring balance of body functions”
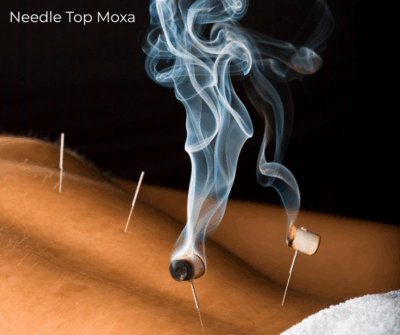
The philosophies and concepts of healing in traditional Chinese medicine are entirely different from conventional or Western medicine. Whereas Western medicine deals with causative agents of disease entities and specific treatments, Chinese medicine adopts a holistic approach, with the aim of maintaining health by restoring balance of body functions. In Chinese medicine, human beings are viewed as part of the universe. The human body, being a small universe, interacts with the environment, the big universe. All that our body takes in (food, air, medication, or stimuli arousing the five senses) are inputs of the outer universe into the inner universe, the human body. According to classical medical texts from China, there are 12 meridians (or primary energy channels) in our body: six yang meridians on the back and six yin meridians on the front. In addition, we have eight extraordinary meridians. It is through these channels that the energy (qi) circulates to every part of the body. Distributed along these meridians are some 360 acupuncture points on the body, all located on the skin, in areas of low electrical resistance and in close proximity to nerve bundles. The principle of acupuncture is to use a needle to stimulate the acupoints in the body to promote the circulation of qi and restore the balance of yin and yang. The therapeutic effect of acupuncture appears at its best when patients have a feeling of special needle sensation (de qi). During “de qi” the underlying muscle appears to grab the needle and hold it firmly. There is propagation of these sensations felt along one or more of the meridians. This theory of acupuncture is unique in Chinese medicine and, to date, there is no logical way to draw parallels with Western medicine.
The effects of acupuncture on gastrointestinal function have been extensively studied by contemporary scientists, mostly reported in the Chinese literature. Unfortunately, the data are difficult to interpret because of the heterogeneity of the study designs and flaws in methodology.3 Scientific studies of acupuncture are further complicated by the fact that needling the same acupoint with different manual skills (pushing or pulling), different frequencies of stimulation, and applied under different basal body conditions may yield totally discordant and sometime contradictory results. The lack of proper control groups in most studies has created another difficulty in the interpretation of data. Unlike testing of new drugs, it is almost impossible to devise a physiologically inert needling procedure that is indistinguishable from real acupuncture. In older studies therefore a proper control group to test treatment efficacy is often lacking. The use of “inert placebo” such as rubbing the needle against the skin or pricking with fingernail have not stood up to criticisms. Recently, several studies have devised improved placebo acupuncture procedures. Lao et al simulated acupuncture by introducing the use of a needle guidetube which blinded the recipient to the treatment.4 Another physiologically inert comparison used in many acupuncture studies is “disconnected” transcutaneous electrical nerve stimulation.5 Yet as the sensations of these placebo procedures are still not identical to real acupuncture, the use of acupuncture naïve patients in single treatment protocols is required to ensure blinding.
“Acupuncture promotes gastric peristalsis in subjects with low initial gastric motility and suppresses peristalsis in those with active initial motility”
Given the limitations of the existing data, animal and human studies demonstrated that acupuncture has certain regulatory functions on gastrointestinal motility and gastric acid secretion. Acupuncture promotes gastric peristalsis in subjects with low initial gastric motility and suppresses peristalsis in those with active initial motility.6 A controlled study also demonstrated that acupuncture reduced basal acid output as well as sham feeding stimulated acid output.7 Inhibition of acid output is not mediated by gastrin stimulated secretion but by the opioid pathway. This is evident by the fact that intravenous injection of the opioid antagonist naloxone prevented the inhibitory effects of acupuncture on gastric motility and acid secretion. However, the acid inhibition effect of acupuncture is transient and diminishes soon after discontinuation of the acupuncture period.7 Animal studies have also demonstrated that acupuncture alters intestinal peristalsis. A high frequency of needle rotation exerts an inhibitory effect whereas low frequency movement actually enhances intestinal motility.8 Unfortunately, the methods used in these studies for measuring intestinal motility were unreliable indices of motor activity. Definitive conclusions cannot be drawn based on existing data. Interestingly, experiments in dogs showed that acupuncturing at Renzhong, an acupoint below the nose above the midpoint of the philtrum, reduced serum levels of 5-hydroxytryptamine (5-HT) and increased 5-HT expression in antral enterochromaffin (EC) cells.9 This finding is intriguing as 5-HT, which is expressed in EC cells as well as in the enteric nervous system, is causally related to the pathogenesis of irritable bowel syndrome.
“Pilot studies have shown that acupuncture is effective in a wide range of gastrointestinal disorders”
Despite the lack of scientific basis, acupuncture has been widely used in the management of gastrointestinal disorders. Uncontrolled data on the clinical use of acupuncture is packed with unjustified enthusiasm. Pilot studies have shown that acupuncture is effective in a wide range of gastrointestinal disorders including nausea and vomiting, functional disorders (irritable bowel syndrome, constipation, and diarrhea), peptic ulcer disease, Crohn’s disease, postoperative ileus, and even gall stone disease. Yet most of these data are anecdotal in nature and unsubstantiated by properly designed randomized studies.10 The most compelling and consistent evidence of the efficacy of acupuncture probably lies in its relieving effects on nausea and vomiting. Vickers et al systematically reviewed 33 randomized controlled trials and found that, overall, the effect of acupuncture was positive.11 However, the antiemetic effect of acupuncture is diminished when administered under anesthesia, suggesting that an intact nervous system is needed for action. A survey from the UK indicated that among common gastrointestinal disorders, patients with irritable bowel syndrome are most likely to seek advice from alternative medicine practitioners and acupuncture is one of the remedies they sought.12 Unfortunately, despite encouraging results from a small scale uncontrolled pilot study,13 subsequent randomized controlled trials failed to substantiate the beneficial effects of acupuncture in irritable bowel syndrome.14
A critical issue in rationalizing the use of acupuncture in clinical conditions is to determine the mechanisms and neuronal pathways of the therapy. Based on existing studies it is likely that somatic afferents primarily convey the input signals of acupuncture to different levels of the central nervous system, including the spinal cord, medulla, mid brain, and subcortex. Both sympathetic and parasympathetic nervous systems relay the impulses to the effectors of the gut via motor and secretory fibres. Opioid peptides play an important role as neurotransmitters in the mediation of acupuncture on gastrointestinal functions. The recent development of functional imaging of the nervous system, such as positron emission tomography (PET) and functional magnetic resonance imaging (fMRI), opens new horizons for studies of acupuncture. Using PET scanning, scientists observed that the thalamic asymmetry present among patients suffering from chronic pain was reduced after undergoing acupuncture therapy.15 Furthermore, it was observed that the “de qi” state of acupuncture was associated with activation of the hypothalamus and cerebellar vermis which was not documented in superficial needling.16 fMRI detects signal changes in the central nervous system in response to stimulation by acupuncture.17 Correlations between acupoints and corresponding brain cortices have been gradually unveiled using fMRI.18
For thousands of years, Chinese medicine and conventional Western medicine appeared to be two unrelated and uncompromising paradigms. Today, we may be seeing light at the end of tunnel using advanced technology to understand ancient healing methods. We should test the validity of acupuncture with the most critical methodology while keeping our minds open. Acupuncture should not be used to compete with efficacious treatment modalities that are already available in conventional Western medicine (for example, proton pump inhibitors for peptic ulcer disease and surgery for appendicitis). Exploration of its clinical applications should focus on conditions for which conventional medicine finds no satisfactory remedy. I believe that as modern biomedical research seriously and enthusiastically explores the potentials of acupuncture, horizons will be broadened for it clinical applications in digestive diseases.
Abbreviations
-
5-HT, 5-hydroxytryptamine
-
EC, enterochromaffin
-
PET, positron emission tomography
-
fMRI, functional magnetic resonance imaging
REFERENCES
1. Dimond EG. Acupuncture anesthesia: Western medicine and Chinese traditional medicine. JAMA 1971;218:1588–63.
2. Capperauld I. Acupuncture anesthesia and medicine in China today. Surg Gynecol Obstet 1972;135:440–5.
3. Li YY, Tougas G, Chiverton SG, Hunt RH. The effects of acupuncture on gastrointestinal function and disorders. Am J Gastroenterol 1992;87:1372–81.
4. Lao L, Bergman S, Hamilton GR, et al. Evaluation of acupuncture for pain control after oral surgery. Arch Otolaryngol Head Neck Surg 1999;125:567–72.
5. Vincent C, Lewith G. Placebo controls for acupuncture studies. J R Soc Med 1995;88:199–202.
6. Yuan CX, Li PM, Zhu J, et al. Clinical value and mechanisms of the action of the acupuncture points “Pishu” and “Weishu”. Chinese Acupuncture 1985;4:5–8.
7. Tougas G, Li YY, Radamaker JW, et al. Effect of acupuncture on gastric acid secretion in healthy male volunteers. Dig Dis Sci 1992;37:1576–82.
8. Yu ZS, Yu YC, Sun ST, et al. The effect of acupuncture at Zusanli with different twirling strengths on small inestinal motility in rabbits. Chinese Acupuncture 1981;1:34–7.
9. Zhou L, Liu LG, Chen HL, et al. The effect of acupuncture “Renzhong” on gastric motility and its relation to peripheral 5-hydroxytryptamine. Chen Tsu Yen Chiu 1987;2:137–8.
10. Diehl DL. Acupuncture for gastrointestinal and hepatobiliary disorders. J Altern Comp Med 1999;5:27–45.
11. Vickers AJ. Can acupuncture have specific effects on health? A systematic review of acupuncture antiemesis trials. J R Soc Med 1996;89:303–11.
12. Smart HL, Mayberry JF, Atkinson M. Alternative medicine consultations and remedies in patients with the irritable bowel syndrome. Gut 1986;27:826–8.
13. Chan J, Carr I, Mayberry JF. The role of acupuncture in the treatment of irritable bowel syndrome: a pilot study. Hepatogastroenterology 1997;44:1328–30.
14. Fireman Z, Segal A, Kopelman Y, et al. Acupuncture treatment for irritable bowel syndrome: a double-blinded controlled study. Digestion 2001;64:1001–3.
15. Alavi L, La Riccia P, Sadek AH, et al. Neuroimaging of acupuncture in patients with chronic pain. J Altern Complement Med 1997;3:S41–53.
16. Hsieh J. Brain activation by acupuncture with “de qi” a PET study. Proceedings of the 4th International Conference on Functional Mapping of the Human Brain, Montreal, Canada, 1998, abstract S440.
17. Wu MT, Hsieh JC, Xiong J, et al. Central nervous pathway for acupuncture stimulation: localization of processing with functional MRI imaging of the brain-preliminary experience. Radiology 1999;212:133–141.
18. Cho ZH, Chung SC, Jones JP, et al. New findings of the correlation between acupoints and corresponding brain cortices using functional MRI. Proc Natl Acad Sci USA 1998;95:2670–3. Retracted
Gut. 2002 Nov; 51(5): 617–619.
doi: 10.1136/gut.51.5.617
PMCID: PMC1773431
PMID: 12377792
Author information Article notes Copyright and License information Disclaimer
This article has been cited by other articles in PMC.